Solutions
You will receive an email with a link to the webinar
Seven essentials of an effective quality management program
The Managed Care Final Rule, along with the shift to value-based care and other industry drivers, is causing organizations across the care continuum to increase their focus on quality management. Implementing a quality management program, however, requires significant change, and lack of structure and attention to key components can result in a lot of work with limited or no results.  Jay Bulot, PhD, has spent the last several years helping states implement quality management programs for Medicaid, aging, and disability agencies. He’s taken his experiences and used them to summarize seven key essentials of an effective quality management program, which he presented in a webinar in October 2018, and which we’ve summarized below.
Jay Bulot, PhD, has spent the last several years helping states implement quality management programs for Medicaid, aging, and disability agencies. He’s taken his experiences and used them to summarize seven key essentials of an effective quality management program, which he presented in a webinar in October 2018, and which we’ve summarized below.
1. Have a clearly defined goal - AIM
In 2008, the Institute for Healthcare Improvement came out with the Triple AIM, a framework for improving health care systems by focusing on individuals to achieve that goal. It was later adopted by the CMS to be the systems approach to improve health care across the United States. The three components of the triple aim were:
The triple AIM has been widely implemented, and it also fits Long Term Services and Supports programs because it has the person at the center, and it also includes all the ancillary services a person might receive, including public health and social services.
Since inception, the focus has expanded to include a fourth component – the clinician experience, which can be defined as including any individual providing services.
The first step in focusing on the Triple and Quadruple AIM is to create an AIM statement. An AIM Statement is:
A clear, explicit summary of what your team hopes to achieve over a specific amount of time, including the magnitude of change you will achieve.
The AIM statement guides your work by establishing what success looks like. Research shows teams who develop a good AIM statement perform better.
2. Agree on the objectives
Once you've created an overarching AIM, you'll want to establish your objectives. What is your quality management program about? As you develop those objectives, you'll want to ensure they follow SMART criteria - that they are Specific, Measurable, Attainable, Reasonable, and Time-bound. Stating a non-SMART objective such as "making life better" makes it difficult to understand if your program is succeeding, which in turn makes it difficult to communicate your success to your stakeholders.
3. Know what to measure
As important as developing goals and objectives is knowing what is important, what is measurable, and what is actionable. Common mistakes, especially those that large agencies often make, include unrealistic expectations about what can and cannot be achieved.
"Just because it can be measured does not necessarily mean YOU can improve it." - Jay Bulot
Work with your stakeholders to determine the best measures on which to focus. Are they appropriate and important? Can they be collected in an affordable fashion? Are they easy to understand?
4. Choose the quality improvement model right for you
There are several quality framework models, including CQI, TQM, Six Sigma, Baldrige, and more. There is no single "right" model, but you do want to use some kind of framework to build structure into your system.
Anything is better than the "Do Nothing" model. In this model, which follows the flow below, improvement initiatives only occur when some external entity forces a change – typically a funder or regulatory agency. 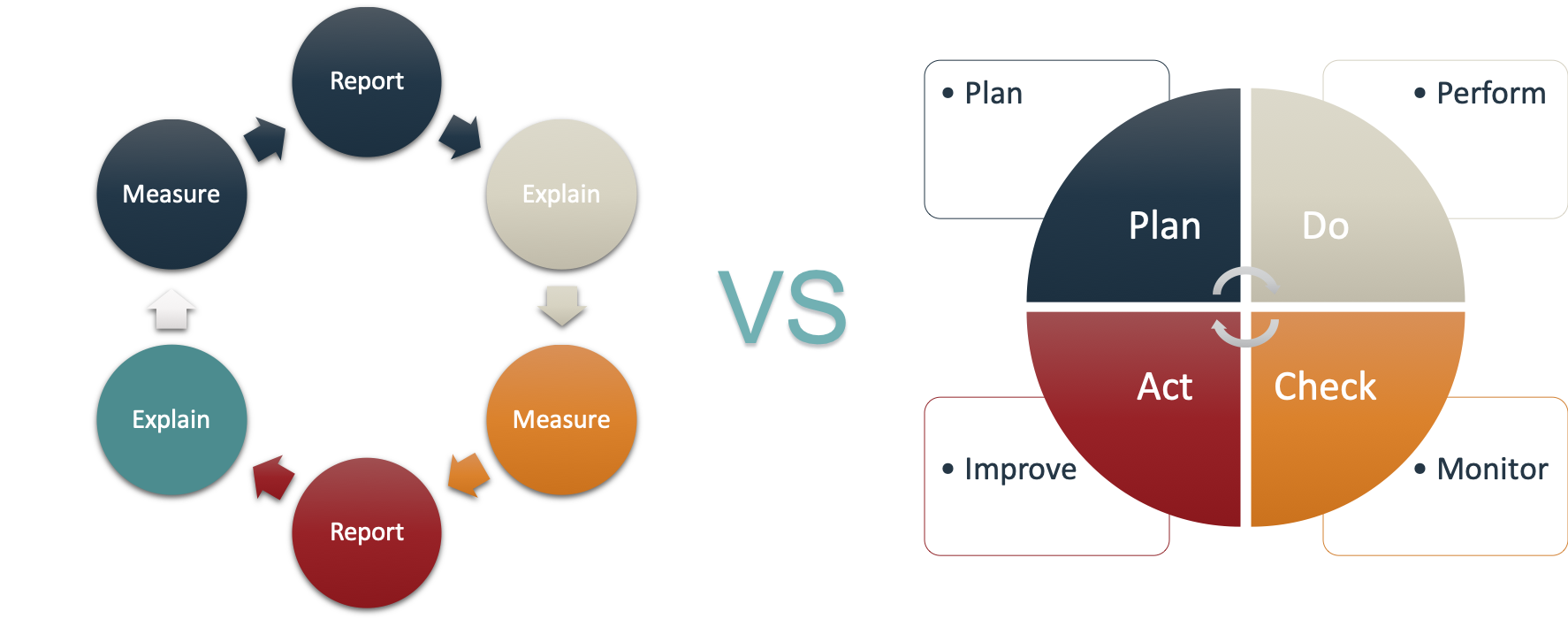
Almost every model has some components of PDCA – Plan, Do, Check, Act. The act of using and striving to improve your programs begins with using your data and making changes to improve.
5. Recognize the potential for value-based purchasing
For many agencies, this could be the first essential element, as it is the move toward value-based purchasing which forces agencies to begin implementing a Quality Management Program. Value-based initiatives, along with the desire to provide better services, are causing providers to reassess their quality programs. In addition, states, managed care organizations, insurers, and others are examining opportunities for value-based purchasing and alternative payment models. Medicare is running several pilots, and most Medicaid Managed Care contracts already have value-based purchasing and alternative payment model requirements.
6. Plan ahead for these common challenges and barriers
Regardless of whether you're a managed care provider, a payer, a care coordinator, or a provider, there are going to be challenges in implementing or improving your quality management program. Mitigate program risks by focusing on the following:
7. Don't Panic. - Douglas Adams
Health care providers have long been under pressure to provide quality care, but this is a relatively new area for those of us working in human services. Don't panic when you start to look at your data and you realize you aren't as good as you thought! Much like driving a car, you rely on the gauges on your dashboard to let you know if you are going too fast, if there are problems, or if you are about ready to blow your engine. 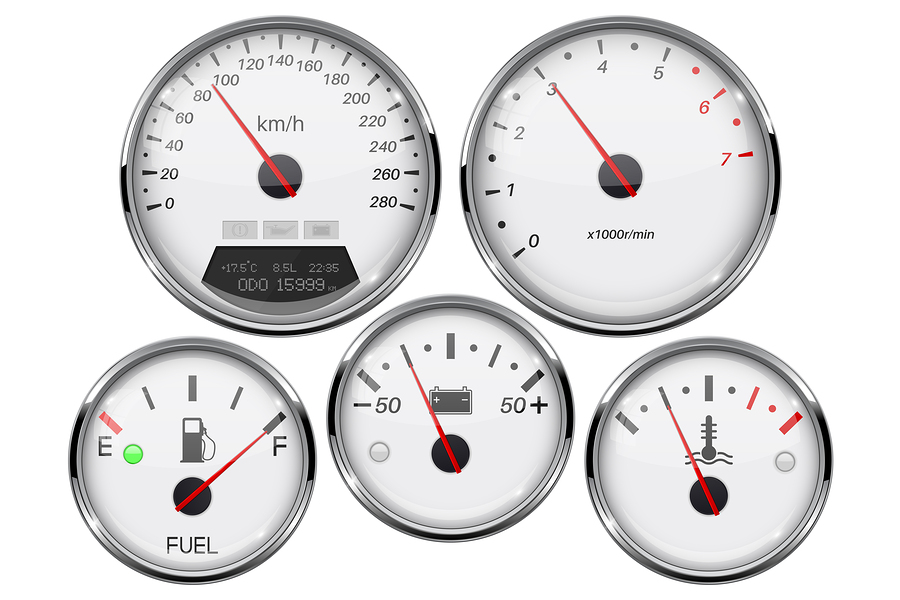 The same is true for program quality. Your data is your dashboard – it tells you whether you are doing well, performing poorly, or if you should hold the course. A quality management program helps you use all the data you have: to make program changes, redirect resources, and to identify other opportunities for improvements to achieve the goals you identified.
The same is true for program quality. Your data is your dashboard – it tells you whether you are doing well, performing poorly, or if you should hold the course. A quality management program helps you use all the data you have: to make program changes, redirect resources, and to identify other opportunities for improvements to achieve the goals you identified.
A strong quality management program in any health care or social services program will ensure you are providing or coordinating the best care possible for your clients or constituents. If you're just getting started, or if you already have a program in place that could use a refresh, review these seven steps and see what you might be missing. Start, or restart your planning processes, review your data, make changes to improve performance, and repeat! Good luck!
Click here to access the full presentation by Dr. Bulot.
Recorded Oct 23, 2018
WellSky only wants to send you the information you are interested in. Please fill out the form below to choose the emails you want to receive. We only send emails to subscribers. If you are an existing customer, you will continue to receive certain notifications.

People who choose a life of caring — and the organizations and communities they serve — deserve a special kind of support. So we help them to care smarter. Liberating them to focus on the people they serve. Providing solutions that make work flow, integrate insights, and update effortlessly.

People who choose a life of caring — and the organizations and communities they serve — deserve a special kind of support. So we help them to care smarter. Liberating them to focus on the people they serve. Providing solutions that make work flow, integrate insights, and update effortlessly.

People who choose a life of caring — and the organizations and communities they serve — deserve a special kind of support. So we help them to care smarter. Liberating them to focus on the people they serve. Providing solutions that make work flow, integrate insights, and update effortlessly.

People who choose a life of caring — and the organizations and communities they serve — deserve a special kind of support. So we help them to care smarter. Liberating them to focus on the people they serve. Providing solutions that make work flow, integrate insights, and update effortlessly.
WellSky is a technology company that delivers software and services to transform an ever-growing range of care services worldwide. We anticipate the needs of care providers and communities, empowering them with insights and solutions that support high quality, scalable, and personalized care. With our platforms and partnership, care providers can deliver their best while managing costs and resources, so both businesses and communities flourish.
Building on a history of excellence and a reputation for quality, WellSky empowers providers to provide exceptional care, improve operational efficiency, reduce cost, and meet the challenges of their rapidly changing industries. Learn more at WellSky.com.

People who choose a life of caring — and the organizations and communities they serve — deserve a special kind of support. So we help them to care smarter. Liberating them to focus on the people they serve. Providing solutions that make work flow, integrate insights, and update effortlessly. So they're able to anticipate — and exponentially increase — the impact of care.
People who choose a life of caring — and the organizations and communities they serve — deserve a special kind of support. So we help them to care smarter. Liberating them to focus on the people they serve. Providing solutions that make work flow, integrate insights, and update effortlessly. So they're able to anticipate — and exponentially increase — the impact of care.
People who choose a life of caring — and the organizations and communities they serve — deserve a special kind of support. So we help them to care smarter. Liberating them to focus on the people they serve. Providing solutions that make work flow, integrate insights, and update effortlessly. So they're able to anticipate — and exponentially increase — the impact of care.

11300 Switzer Road, Overland Park, KS 66210
855-935-5759
© Copyright 2025 WellSky. All rights reserved.